Estimated readtime: 7.5 min
This blog was written by Sherine Guirguis, Co-Director of Common Thread, and originally appeared on Common Thread’s Medium blog.

By Sherine Guirguis, Co-Director of Common Thread
Common Thread puts people at the centre of Public Health. Find us at: gocommonthread.com
“I’m pretty sure I had Covid last October. I never get sick, and this was bad. I couldn’t go to work for 3 days. I don’t need the vaccine. I’ve already got the antibodies.”
That’s my Uber driver, Terell, telling me why he feels safe shuttling people around every day. And why he won’t be taking any Covid vaccines when they come out. Terell is African American, which statistically makes him 5 times more likely to be hospitalised with Covid. His wife has Diabetes. And although he hasn’t been tested for antibodies, he doesn’t think a vaccine will give him any more protection than he already has. As for his wife, the fact that she never got infected, even throughout his own “illness”, is just a testament to her incredibly strong immune system.
The rumour mill around Covid-19 has been vibrant, no matter where in the world you live. Rumours and perceptions that circulate in Bucharest, where I live, are almost identical to the ones I heard this summer in New Jersey, where I met Terrell. Most people I have encountered on both sides of the Atlantic believe Covid-19 is real — they just think the Government or the Scientists have exaggerated its prevalence for political gain. Friends and family members in the US told me the same stories as swim instructors and teachers in Romania. “A family friend passed away last week, but he died of a heart attack and the hospital classified his death as Covid-19.” I have heard variations of this one numerous times. “They’re just trying to get the numbers up.” “We went out last night without masks and everyone’s fine this morning.”
A WAR ON TWO FRONTS
Covid-19 is the perfect storm for misunderstanding, rumours and fake news. The disease is new, it’s invisible, unpredictable, and its progression feels out of our control. Adding fuel to the misinformation fire, most public health advice throughout the pandemic has been confusing and overwhelming.

People are home, surfing the web and communicating via WhatsApp and social media, trying to fill in the gaps. While most of this web-surfing and social media sharing is rooted in genuine searches for information, the phenomenon has exacerbated what behavioural scientists call ‘Group Polarisation.’
Essentially, people will find the views they’re looking for online and once in the company of similar minded people, become more extreme in their views, even if they’re incorrect.
The situation is so widespread that the World Health Organization has given it a new name. An Infodemic is ‘an overabundance of information — some accurate and some not — rendering it difficult to find trustworthy sources of information and reliable guidance.’
“We’re not just fighting a pandemic; we’re fighting an infodemic” — WHO’s Director General, Dr Tedros Ghebreyesus.
So it’s really quite logical that the next stop on the Covid-19 infodemic train is the imminent Covid vaccine. Many people are anxiously awaiting the vaccine, pinning their hopes for “normalcy” to its rapid release. For others, the Covid vaccine is just the latest prevention tactic that seems politicised, confusing, and potentially more hassle than it’s worth.
COVID IN THE TIME OF HESITANCY
The hesitancy towards a Covid vaccine is an indicator that vaccine hesitancy — once reserved for fringe anti-vaxxer groups — is now moving into the mainstream.
“A lot of people you never would have imagined are now saying that maybe the anti-vaccination lobby has a point.” – Heidi Larson, Director of the Vaccine Confidence Project at London School of Hygiene and Tropical Medicine.
In April, a social media campaign #africansarenotlabrats trended fast and wide across social media channels, signalling a loud declaration from African citizens that they would not be testing the vaccine for the rest of the world. Protests continue in Africa against Covid vaccine trials, demanding that a long history of medical experimentation end now.
In the US, recent polls suggest that as few as 50% of Americans plan to get a Covid vaccine. A survey in the UK found that only 30% of British people are positive they’ll take the vaccine.
A vaccine has myriad benefits. But Covid-19 will be difficult to contain and stamp out if large portions of the world’s population won’t take a vaccine.
So what can governments do in the face of this unprecedented resistance to the only viable medical solution on the table?
Here are five suggestions that could potentially end the pandemic:
All of these things can and should be done now, before a vaccine has even been released.
1. Focus on the positives:
Find the people who have clearly said “yes” to a vaccine now — and make sure they get vaccinated. For this group of early adopters, policy makers must do everything possible to move their intention to action.
As Common Thread knows from research on broader vaccine acceptance, resistors are hard to budge, though it is tempting to tackle them first. But trying to sway this group will not yield great benefits. Policymakers should simply try to limit their influence.
Focus strongly on getting a vaccine to everyone who wants it. For the ‘wait and see’ group who will be watching for more evidence once the vaccine is in the market, make sure the case for efficacy and safety is clear and incontestable. They are likely to come around.
2. Make it easy:
Studies of annual flu vaccination campaigns show that even people who intend to get the flu jab often don’t get around to it because…well, life kicks in. To make sure life doesn’t get in the way of Covid vaccination, health officials can help make sure that people who want to get vaccinated don’t procrastinate, forget, or get caught up in a Zoom fog on their way to a clinic.
Public Health Managers can adopt behavioral science’s “make it easy” mantra to Covid vaccination. Set up clinics in workplaces, pharmacies, public areas, shopping malls and other community gatherings. Making it easy also has an added benefit of making it visible — helping to further cement vaccination as something everyone is doing.
3. Put people at the centre of the vaccination effort:
As we know from previous outbreaks, people respond to risk in dramatically different ways. Context, income, education, culture, social norms, and competing risk all play a huge role in determining how people will respond and comply with health advice. These variables and their priorities are constantly shifting.
For policy makers who are just trying to stay on top of the latest scientific evidence, people’s behaviour can seem like an unpredictable black box of obfuscation. But people — if engaged and employed as partners — can be powerful assets to leverage in an outbreak.
Dr. Mike Ryan, WHO’s Executive Director of Health Emergencies is a Common Thread hero for combining empathy with sound public health strategies that promote real community engagement and dialogue.
4. Speak the (emotional) lingo:
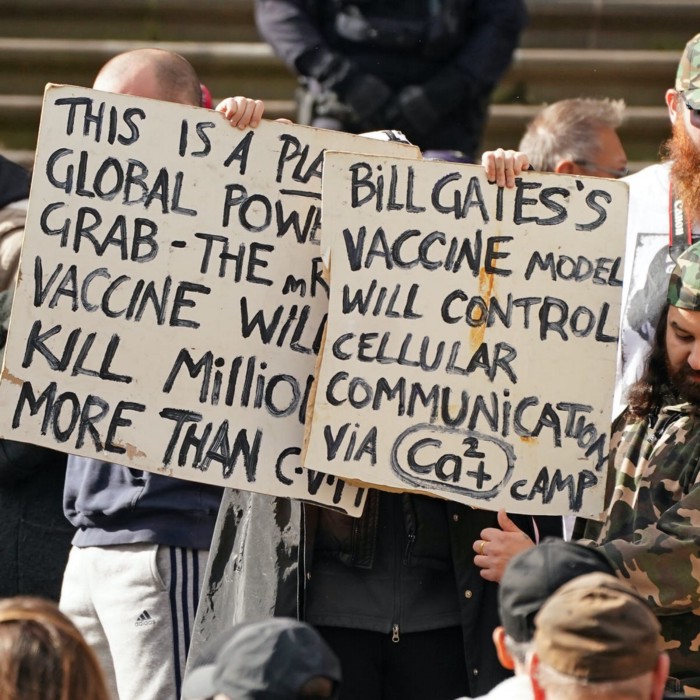
The anti-vaxxing narratives are diverse, creative, and widespread. Their angles range from safety, to the perils of capitalism, to the benefits of alternative medicines, to immunization as a conspiracy theory. Other hesitancy narratives for Covid vaccine play to people’s genuine concern over the speed of vaccine development.
Regardless of the content, anti-vaxxing narratives employ personalised, strategically-placed messages that tap into people’s emotions. By contrast, pro-vaccine groups generally have one simple message: vaccines work and save lives.
Public health campaigns often employ dry medical facts and stick to traditional channels to get their message out. To drown out the anti-vaxxing narrative, the alternative needs to be stickier, more creative, more emotional, and more widespread. People remember good stories that make them feel things. With hundreds of thousands of lives and jobs lost to Covid, and so much more at stake, there is no shortage of emotional fodder for the Covid vaccine story. Policymakers need to leverage it.
5. Design for women:
Women form 70% of the global health workforce, but are “underrepresented in leadership positions, clustered into lower-status, lower-paid jobs and commonly subject to harassment.” Across the world, women and girls perform more than 75% of total unpaid care work, making them most likely to serve as the primary caregivers for family members who have been affected by Covid.
In the United States, women make approximately 80% of family health decisions. Yet health programmes and emergency response plans are primarily designed by men, for other men. Want to ensure people take the Covid vaccine? Convince women it’s a good idea, and then help them secure it for their families.
This means placing women at the top table of strategy and programme design, and understanding what they need to make the right choice.
“The pandemic has finally opened our eyes to the fact that health is not driven just by biology but by the social environment — and gender is a major part of that.”
And Finally…
The history of pandemics and how they ended has demonstrated that humanity has so far prevailed when facing a challenge on a global scale. But the world didn’t have the internet in 1918 during the Spanish Flu. We didn’t have organised anti-vax movements, or legitimate looking social media feeds.
Arguably, there wasn’t such distrust in public health organisations when childhood vaccinations for Polio, Measles, Mumps or Rubella first became available. Human behaviour is what is spreading this deadly, raging virus. It should be a given for people to be at the heart of our future solutions to consign Covid-19 to history.
